This blog post was written by PhD student Nicola Rea. Nicola’s PhD ‘Improving care transitions for critically ill patients’ requires access and use of National Safe Haven Data for data analysis. Nicola writes about her experience below.
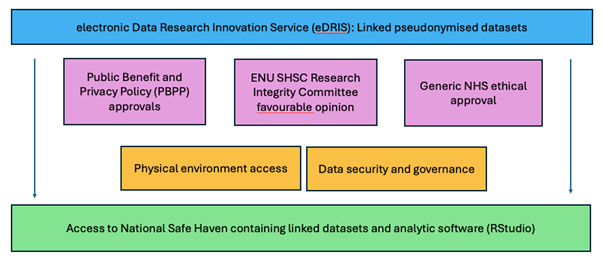
Over the last two decades, National Safe Havens (NSH) have become ubiquitous in healthcare data research. The term “Safe Haven” covers two fundamental functions – a physical environment containing linked datasets and governance procedures to ensure sensitive data is managed in a secure manner. This study, carried out as part of my PhD sought the use of routinely collected data, which is pseudonymised at the point whereby researchers access the data and permitted the analyses of a national cohort of patients in Scotland.
This study aimed to understand the long-term outcomes for critical care survivors with pre-existing cardiovascular disease, an under-researched area whereby the answers remain unknown. The specific research questions are as follows:
- Does pre-existing cardiovascular disease influence hospital readmission (within one year of index hospital discharge) rates?
- What is the prevalence of pre-existing co-morbid disease in the Scottish ICU population?
- What is the prevalence of pre-existing CVD in the Scottish ICU population?
- Does pre-existing CVD influence whether patients are discharged home following an ICU admission?
- Does pre-existing co-morbid disease influence whether patients are discharged home follow an ICU admission?
This study was carried out as part of a wider National Health Service (NHS) project which had previously sought and been granted both Public Benefit and Privacy Policy (PBPP) approval and generic NHS ethical approval. For me to gain access to the linked data held in the Safe Haven as part of this wider project, completion of Medical Research Council (MRC) Research, Confidentiality and GDPR training was required. On completion I was added as a “User”. Approvals were also sought and granted from Edinburgh Napier University (ENU) School of Health and Social Care (SHSC) Research Integrity Committee.
As a PhD student, I carried out extensive training in both statistical analysis and RStudio data analysis software. The analysis presents both descriptive and inferential statistics to answer the research questions outlined above. More specifically, binary logistic regression models have been developed to determine if CVD is a predictor of hospital readmission (within one year of index hospital discharge) or to determine discharge destination for patients with CVD or non-CVD co-morbidities. The findings from this study are required to undergo review by the electronic Data Research Innovation Service (eDRIS) for statistical disclosure prior to removal from the NSH. Until then, we are unable to share the results but hope to do so in the coming weeks.
If you would like to know more about this study, please contact myself, Nicola Rea (Nicola.Rea@napier.ac.uk).
The NSH accessed for use in this study is managed and maintained by eDRIS (part of Public Health Scotland).